Efficient Billing Solutions for Large Practices
Billing errors can hinder your large practice’s financial growth. With 10+ years of expertise in billing and denial management, Apex Precision Billing reduces claim denials by 97% and recovers lost revenue. Serving all 50 states!
Apex precision billing & Large Practices – Aligned for Success!
Accelerate Cash Flow &
Boost Revenue
Compliance Regulation
Cost Savings
Precision in Billing & Coding
Enhance Patient Experience
End-to-End Denial Management
Strong Billing Infrastructure – A Key Advantage of Our Medical Billing Services
Large practices face numerous challenges, from patient registration to claims submission and follow-ups, with filing multiple claims being a major hurdle.
A strong billing infrastructure brings transparency, affordability, and flexibility, refining weak areas in the billing process. That’s where Apex precision billing excels. Our advanced systems, equipped with up-to-date denial management tools and expert personnel, ensure seamless solutions and 24/7 support.
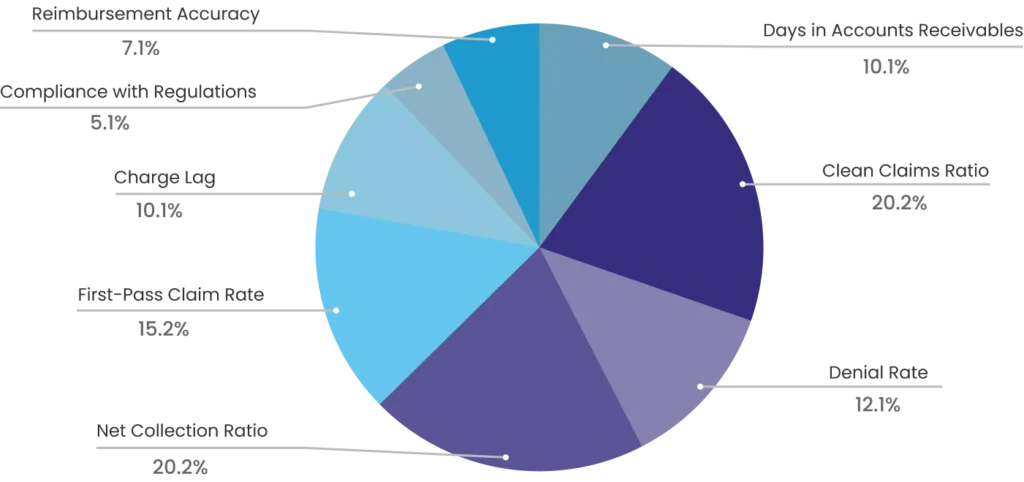
8 Key KPIs to Accelerate ROI and Boost Revenue
These key metrics form the backbone of the revenue cycle management flowchart, optimizing the billing process and financial performance of your large practice.
We Use 4 Key Metrics to Audit Billing & Optimize ROI for Your Large Practice
These metrics account for 60% of your billing process’s efficiency, productivity, and financial performance—backed by real client data and experience.
Days in Accounts Receivable - 30-40 days
Accounts receivable is the process of tracking claims buy considering the average number of days practice takes to collect due payment. We have lower accounts receivables days ratio and ensure faster reimbursement
First Pass Acceptance Rate - 97%
Also known as the first pass clean claim rate, it measures the acceptance rate of the first submission of the claims. We provide quality revenue cycle management services for a high first-pass clean claim rate.
Net Collection Rate - 98%
The overall collection from the patient and the insurer makes the net collection rate. We make sure payment is timely received and the net collection rate is high.
Denial Rate - 1%
The ratio of claims denied by the insurer represents how effective is your revenue cycle management process. We follow up on denied claims, scan, and rectify the errors and maximize revenue generations.
Medical Billing Services to Optimize Revenue Cycle Management for Large Practices
Simplify medical billing complexities and boost financial and operational efficiency with this streamlined billing flowchart for your large practice
Insurance Verification & Eligibility Check
Secure prior authorization and verify insurance eligibility for diagnoses, procedures, and treatments.
Seamless Patient Registration Process
Collect, verify, and enter the data into the system to ensure accuracy and error-free billing documentation.
Efficient Claims Submission
With a 99% clean claim rate, we ensure accurate submissions for a high first-time pass rate and maximum collections.
Precision Coding & Documentation
Our expert coders and billers ensure precise diagnostic and procedural coding, minimizing errors and inaccuracies.
Effective Denial
Management
Rectification of the root cause of the denial leads to accuracy and successful denial management.
Accurate Payment Posting
Record and post payments from insurers or patients, ensuring accurate tracking and co-pay notifications.
01
Seamless 24/7 Technology & Resources
Leverage cutting-edge billing technology, coding tools, and robust infrastructure to streamline operations and customize billing & RCM for large practices. With BellMedEx, outsourcing your billing means accessing these advanced resources without the expense of software or hardware.


02
Continuous Auditing for Unmatched Quality
We conduct regular internal audits to identify inaccuracies and highlight areas for improvement in billing processes. Additionally, we correct recurring patterns and implement strict quality control measures, including double-checking claims and thorough reviews. This ensures accuracy and minimizes revenue losses.
03
Transparent & Proactive Communication
Transparent and efficient communication among insurers, administrative staff, and billing teams is key to building strong, long-term partnerships. It fosters trust, minimizes misunderstandings, and reduces errors for smoother operations.


04
Expertise and Specialization
Experience and professionalism are key metrics to ensure fewer denials. We have a team of trained experts skilled in coding, billing, and claims submission. Your large practice can tap into this knowledge to access compliant billing practices.
05
Simplifying Complex Coding System (ICD-10, CPT, HCPCS)
We stay updated with the latest regulatory changes, coding guidelines in diagnostic procedures, and insurance requirements and employ coders who are well-versed in ICD-10, CPT, and HCPCS coding systems to ensure accuracy and faster collection.


